Introduction
The treatment of polycystic ovary syndrome is closely related to the severity of the symptoms, the type and/or extent of the hormonal alteration present in the plasma and, above all, to the presence or absence of the woman’s desire for pregnancy.
In practical terms, the therapeutic intervention is aimed at controlling menstrual cyclicity and/or dysfunctional bleeding, reducing the clinical signs of hyperandrogenism and improving metabolic aspects.
Today, new non-pharmacological approaches have been introduced in the management of the syndrome. Inositol is commonly taken with food, but the sufficient amount taken by healthy subjects is not enough for those who suffer from specific diseases, such as PCOS.
The search for inositol and the ever-deeper knowledge of PCOS leads today to be able to say that myo-inositol represents a key element.
In this article we will analyse precisely what the results of myo-inositol-based therapies on the polycystic ovary are.
What is Myo-inositol
Myo-inositol is a chemical compound widely spread in plants: green beans, peas, asparagus, walnut leaves, grape, pears, cherries, apples, tomatoes, yeast, carrots extract. In oats, maize, and cereals it is generally present as a component of lecithin, in the form of inositol-6-phosphate or phytic acid.
In animal tissues, it is abundantly present above all in the brain and muscles. High quantities of myo-inositol are present in the sperm, oocyte and embryo during the early stages of embryonic development.
Myo-inositol acts as the second messenger of the hormone-insulin, FSH and TSH.
But what does “second messenger” mean?
If you think of a relay race, the second messenger is just like the second runner who takes the baton from the first athlete (who in our case is a hormone) and transfers it to the third athlete who will take him to the finish. Understood that, if the second messenger is missing, there will be no response to the first signal (no victory).
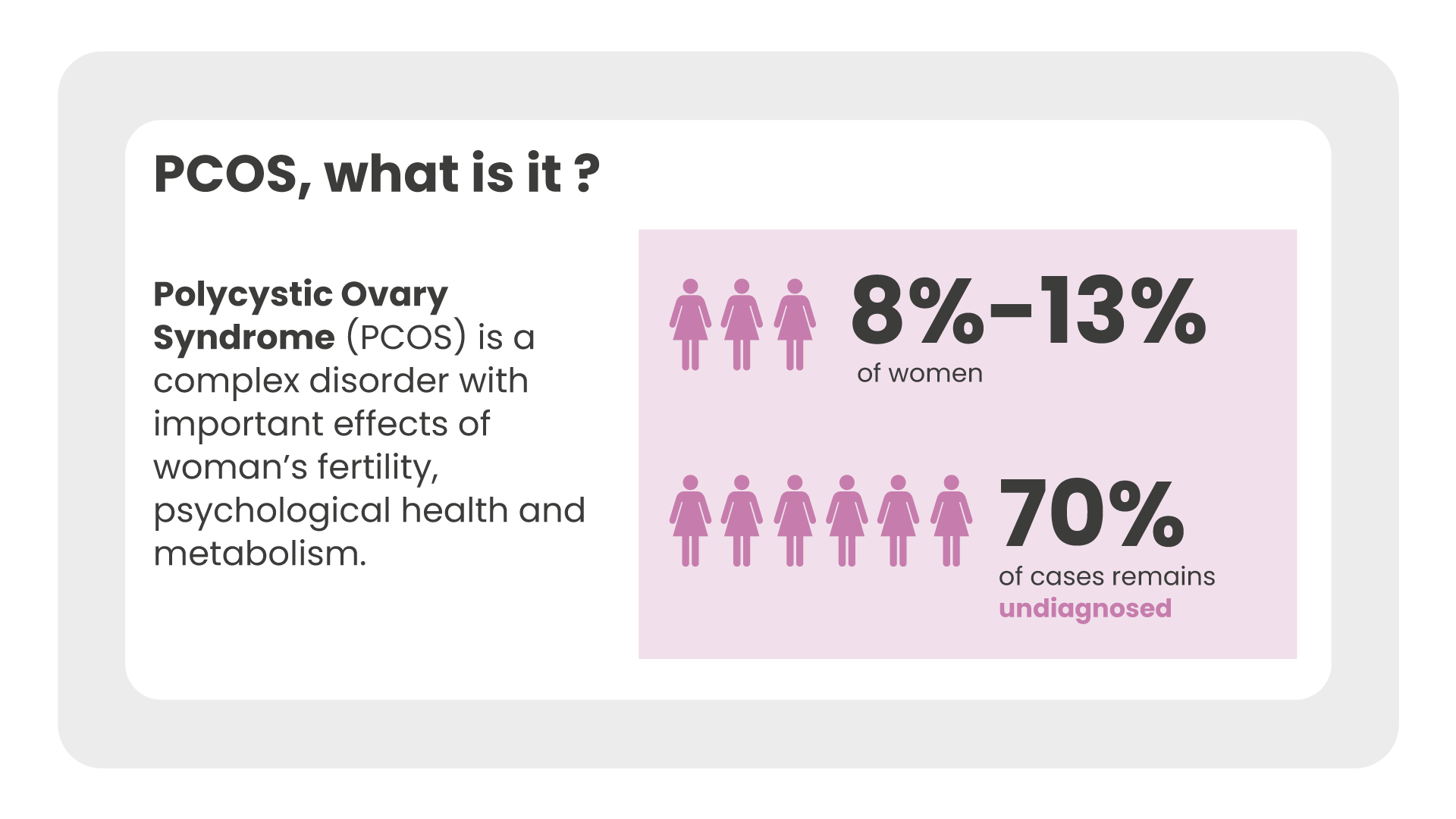
PCOS: what it is and how it is diagnosed
It is a multifactorial disease that affects about 5% -10% of women of reproductive age, regardless of their ethnicity. It causes important aesthetic, metabolic and reproductive effects on women’s health and the aetiology is still controversial today.
- clinical and / or biochemical hyperandrogenism.
- ovarian dysfunction;
- polycystic ovaries on ultrasound examination, with at least 20 follicles with a diameter of less than 10 mm and increased ovarian volume.
Therefore, to make a diagnosis of PCOS it is necessary not only to perform an ovarian ultrasound but also a series of biochemical investigations: measurement of male hormone levels, the FSH / LH ratio, control of metabolic parameters (blood sugar and insulin).
Symptoms can vary from woman to woman and, if not properly treated, PCOS can lead to more serious complications, such as type 2 diabetes, cardiovascular disease and infertility.
The causes of PCOS
It can be said that PCOS is the expression of a complex functional alteration of the reproductive system given by the increase in male hormones, the cause of signs and symptoms such as: amenorrhea, hirsutism, but also weight gain due to insulin resistance.
In most cases, affected women do not know that this pathology originates from a metabolic dysfunction that leads to gynecological complications, such as absent or irregular menstrual cycle, lack of ovulation and infertility.
PCOS therapies
A change in lifestyle, aimed at promoting weight loss, must always be suggested to PCOS women who are overweight, representing a safe and cheap initial approach to try to improve the reproductive function and metabolic profile of these patients [2] . PCOS should not be considered only as an exclusive disorder of women at childbearing age, but as an endocrine-metabolic disorder with important long-term health implications.
PCOS, as a syndrome, requires adequate medical interventions to control all the alterations connected to it.
The problem that for years has made diagnosis and therefore also the cure of PCOS difficult is that there is no homogeneity of symptoms. However, to give an overview of the clinical manifestations and risks of women with PCOS, we can divide them according to age groups.
Myo-inositol and its benefits for PCOS
Several clinical studies have shown that the constant intake of myo-inositol is able to restore both ovarian and metabolic function [3] [4].
A recent meta-analysis [3], which examined a series of studies involving a total of 247 women with PCOS treated with myo-inositol and 249 controls, showed that treatment with myo-inositol:
- significantly decreases levels of insulin, HOMA-index and androgen (free testosterone);
- while it increases those of the sex hormone binding globulin (SHBG).
Previously, another review [4] had provided evidence that inositol significantly improves the rate of ovulation and regulates the frequency of menstrual cycles.
As for PCOS, studies have shown the efficacy of this molecule with the intake of 2g of myo-inositol twice a day (for a total of 4g) for the powder formulations (sachets, tablets).
In addition to the importance of dosages, studies highlight two other key elements for the effectiveness of myo-inositol.
The first is the intake, for the powder formulations, away from meals in order not to interfere with their absorption. Second administration is given during the day.
Kinetic studies have shown a 12-hour half-life of inositol [5]. By using double administration, better coverage of the insulin response is obtained.
Conclusions
In conclusion, the observations emerging from the numerous studies suggest that inositol represents an effective therapy in the treatment of patients with polycystic ovary syndrome.
Myo-inositol also plays a specific key role in reducing serum testosterone levels and in controlling insulin levels.
Given these premises, inositol is useful in preventing and correcting the pathophysiological mechanisms underlying the metabolic alterations that cause PCOS.
Sources
[1] Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004 Jan;81(1):19-25.
[2] Le Donne M. Effects of three treatment modalities (diet, myo-inositol or myo-inositol associated with D-chiro-inositol) on clinical and body composition outcomes in women with polycystic ovary syndrome. Eur Rev Med Pharmacol. 2019 Mar;23(5):2293-2301.
[3] Unfer V. Et al. Myo-inositol effects in women with PCOS: a meta-analysis of randomized controlled trials. Endocr Connect. 2017 Nov;6(8):647-658.
[4] Pundir et al. Inositol treatment of anovulation in women with polycystic ovary syndrome: a meta-analysis of randomised trials. BJOG. 2018 Feb;125(3):299-308.
[5] Monastra et al. Alpha-lactalbumin effect on myo-inositol intestinal absorption: in vivo and in vitro. Curr Drug Deliv. 2018;15(9):1305-1311.